When Henry Ford famously wrote in his autobiography that “Any customer can have a car painted any color that he wants so long as it is black,” he was responding to a frustration and an opportunity.
The frustration was with his sales people who, in 1909, were constantly trying to improve sales by appeasing the design whims of a few customers (those customers, that is, who could afford it).
The opportunity was that he’d been experimenting with a fast-drying paint that helped speed up the assembly line – and that newly developed paint was only available in black at the time.
The Model T was the car in question — and had been available since 1908 in fire engine red and hunter green, as well as black.
One Message, One Voice, One Paint Color
HR and benefit managers often feel like they’re under an edict that they can only use black paint. That is, the rules that shape the company’s brand and its external communications are applied to internal employee communications – and often get in the way of effective benefit messages. Corporate firewalls prevent benefit information from getting easily to employees’ families. Policies that state all communication with employees will be in English fail to take into account those who can more readily understand another language, and thus be in a better position to make good use of their benefits. Sometimes even the tone of voice governed by Corporate Communications can defeat the effectiveness of a message: when was the last time a corporate style guide allowed the use of humor?
“Today, to be effective, branding messages need to be less about the organization and more about the interests and needs of the target audience,” says Marvin Smith of Lockheed Martin. “It has created an unprecedented transparency into an organization’s culture, people and processes as we have moved to a state where ‘it is not about us, it is about them.’”
The policies, rules, guidelines, and templates used in branding content for customers and for internal communication have been well thought through. As David Kippen, CEO of Evivva Brands, puts it, “A great employer brand goes further. It connects, people, passion and purpose. It does this by describing something honest and true at the intersection between what people do, the company’s purpose, and what the company uniquely enables. And when it has that message in the crosshairs, it aligns the organization around it: one message, one voice, inside and out.”
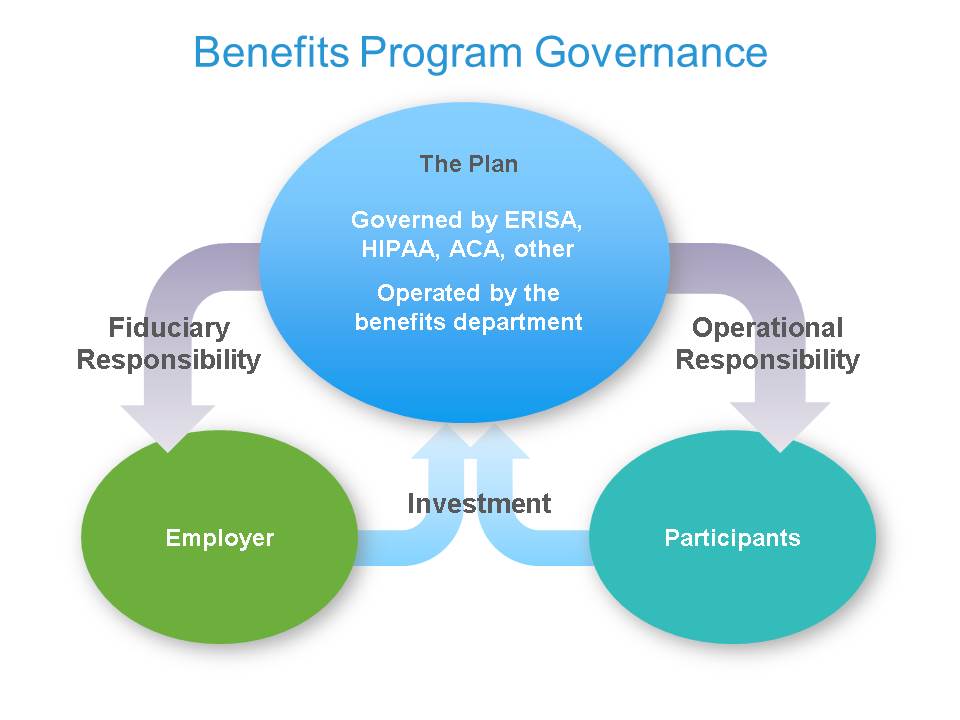
Yet that “one message, one voice” can be a serious drawback when it comes to benefits information. Organizations need to stop thinking of their benefits audience as employees, and start thinking of them as plan participants—an audience that includes employees, spouses and partners, adult (and perhaps child) dependents, plus retirees, COBRA participants, and so on. This audience—or more to the point, audiences—requires different rules, poses different challenges, and has different expected outcomes. Because HR specialists manage and are responsible for the outcomes of the benefit programs, they are fiduciaries in a system that has – and needs – its own rules of communication.
[ctt title=”Stop thinking of your benefits audience as employees & start thinking of them as plan participants ” tweet=”Stop thinking of your #benefits audience as employees & start thinking of them as plan participants http://ctt.ec/fctpa+ @XeroxHRInsights” coverup=”fctpa”]
Access Restricted
For instance, to overcome barriers to information access, some employers implement a benefits or HR website. But often these portals are secured behind a firewall to accord with corporate policy on the privacy and protection of internal communications.
But then how can a retiree, a remote-working employee, and the employee’s family get to that same information? Benefits managers know that effective utilization of health care and prescription drug benefits rely on providing timely, regular benefits communication to guide and encourage wise use of the programs: the retiree needs information on medication (and, like everyone else, needs to be reminded to follow the prescription properly); the employee who needs to follow a physiotherapy treatment plan wants the best information on practitioners and outcomes; and the employee’s spouse with a serious medical condition needs to know of alternative treatments covered by the benefits plan. A corporate policy that hides access to this information behind its firewall is only going to cost the company in the long run as expensive pharmaceuticals, missed therapy sessions, and less-effective treatment plans help to raise health care costs.
A Picture is Worth a Thousand Words – But Only in English
Another common corporate guideline, especially in organizations with a broad global workforce, is the one that says communication will only be in English. Yet benefits communication often needs to be explained in other languages. The health care field is strewn with jargon, terms and concepts that are hard enough to understand in English. Helping a sector of the workforce that’s more comfortable in a different language helps improve the results (and lowers the cost) of medical treatments.
Finally, the visual appeal of benefit communication too often runs head-on into the corporate guidelines concerning the design of the messages. Brand rules that forbid cartoons (cartoons that often help with language and terminology barriers to understanding), or that allow only stock photographs based on its industry as visuals in a benefit communications piece, are themselves barriers to effective messages. If yours is a hi-tech industry, chances are all the stock photos available are of younger employees – how could a retiree “see themselves” in the picture?
Break the Rules?
So what should the HR/Benefits Manager do?
[ctt title=”What should HR do when your company\’s brand gets in the way of effective benefits communication? ” tweet=”What should #HR do when your company’s brand gets in the way of effective #benefits communication? http://ctt.ec/id8Ij+ @XeroxHRInsights ” coverup=”id8Ij”]
Mike Natalizio, president and chief executive officer of HNI, looks at it this way: “Employers need to rethink their whole benefits communication strategy. They need to determine what to say, who needs to hear it, and how to deliver it. These factors are critical to effective communication, because employees today are more skeptical as they see their benefits decreasing and their premiums rising. As employers begin to provide information about health care reform measures, employees are going to have their radar up,” he says. “They’re going to be saying, ‘Okay, here it comes. How much more of the cost are they going to shift over to me?'”
The fact is, as Benefits Manager, you need to make the case that your “constituency” – participants in a benefits program – need different communication styles that sometimes break the usual corporate style rules.
Organizations that have been willing to bend — sometimes even “break” the rules of corporate communication — have realized significant returns. These include such results as:
- Participation rates in wellness and disease management programs that are at least double the norms
- Meaningful improvements in health status across the entire plan population, and
- Greater employee satisfaction with their benefits.
Better still, some plan participants may even want to engage more with their benefits, and their benefits information. For example: One employer who produces an annual wellness calendar has learned to print numerous extras as employees request two or more copies: one for the office, one for home, and an extra one for their spouse.
Now, when was the last time anyone wanted an extra copy of your benefits communications?