Many of us are COVID-19 weary, yet the pandemic persists, and the virus continues to spread. The number of new COVID-19 cases in the United States last week rose 18% to more than 575,000, while the number of tests performed rose 5.5%, according to a Reuters analysis of state and county reports.
Nationally, over 5,700 people died of the virus in the seven days ended November 1, bringing the total to over 230,000. Thirty-four out of 50 states have seen new cases increase for at least two weeks in a row, down from 36 the prior week.
Sources: https://www.healthline.com/health-news/here-are-the-states-where-covid-19-is-increasing and https://graphics.reuters.com/HEALTH-CORONAVIRUS/USA-TRENDS/dgkvlgkrkpb/index.html
According to Johns Hopkins University, as of November 5, 2020, the Coronavirus SARS-coV-2, has infected more than 48 million people worldwide (more than doubling numbers since August 2020) and killed more than one million people.
Source: https://coronavirus.jhu.edu/us-map
Testing update
There are two different types of tests: diagnostic (molecular and antigen) and antibody.
A diagnostic test can reveal whether you have an active coronavirus infection and you should isolate yourself from others. An antibody test may indicate whether you have had the virus. At this time, researchers do not know if the presence of antibodies means that you are immune to the coronavirus in the future.
New tests are coming onto the market on a regular basis. Some may decrease the wait time to receive results. The graph below, sourced from the CDC, may help answer testing questions.
| Molecular test | Antigen test | Antibody test | |
| Also known as… | Diagnostic test, viral test, molecular test, nucleic acid amplification test (NAAT), RT-PCR test, LAMP test | Rapid diagnostic test (some molecular tests are also rapid tests) | Serological test, serology, blood test, serology test |
| How the sample is taken… | Nasal or throat swab (most tests), Saliva (a few tests) | Nasal or throat swab | Finger stick or blood draw |
| How long it takes to get results… | Same day (some locations) or up to a week | One hour or less | Same day (many locations) or 1-3 days |
| Is another test needed…
|
This test is typically highly accurate and usually does not need to be repeated. | Positive results are usually highly accurate but negative results may need to be confirmed with a molecular test. | Sometimes a second atibody test is needed for accurate results. |
| What it shows… | Diagnoses active coronavirus infection. | Diagnoses active coronavirus infection. | Shows if you’ve been infected by coronavirus in the past. |
| What it can’t do… | Show if you ever had COVID-19 or were infected with the coronavirus in the past. | Definitively rule out active coronavirus infection. Antigen tests are more likely to miss an active coronavirus infection compared to molecular tests. Your healthcare provider may order a molecular test if your antigen test shows a negative result but you have symptoms of COVID-19. | Diagnose active coronavirus infection at the time of the test or show that you do not have COVID-19. |
Types of diagnostic tests
There are some new diagnostic tests available with alternative methods and benefits.
| Rapid, point-of-care diagnostic tests use a mucus sample from the nose or throat but can be analyzed at the doctor’s office or clinic where the sample is collected and results may be available in minutes. These may be molecular or antigen tests. | At-home collection tests, available only by prescription from a doctor, allow the patient to collect the sample at home and send it directly to the lab for analysis. | Saliva tests allow a patient to spit into a tube rather than get their nose or throat swabbed. Saliva tests may be more comfortable for some people and may be safer for healthcare workers who can be farther away during the sample collection. |
No test is 100% accurate all of the time. Some examples that may affect the test’s accuracy include:
- You may have the virus, but the swab might not collect it from your nose or throat
- The swab or mucus sample may be accidentally contaminated by the virus during collection or analysis
- The nasal or throat swab may not be kept at the correct temperature before it can be analyzed
- The chemicals used to extract the virus genetic material and make copies of the virus DNA may not work correctly
The best way to get a coronavirus test is to contact your health care provider. You may also visit your state or local health department’s website to look for the latest local information on testing.
Source: https://www.fda.gov/media/140161/download
Vaccine update
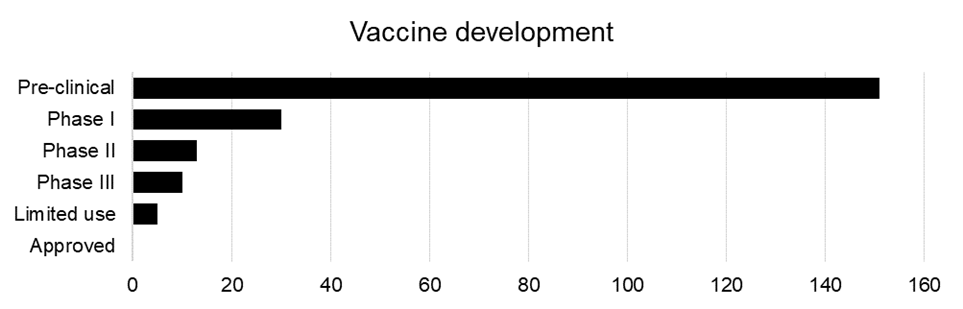
Currently, there are 209 vaccines in various stages of development.
Source: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
There has been speculation that a vaccine may be available as early as the beginning of 2021, but even then, there are unknowns. In June, the Food and Drug Administration (FDA) published guidelines requiring that the vaccine trials were at least 50% effective. Depending upon how many people are willing and able to receive the vaccine once it is ready for distribution and the efficacy of the vaccine, it may leave significant populations unprotected.
Source: https://www.fda.gov/media/139638/download
Updates from the Centers for Disease Control (as of October 28, 2020)
The Centers for Disease Control (CDC) issued updated guidance to its How COVID-19 Spreads website, which includes information about the potential for airborne spread of the virus that causes COVID-19.
The CDC continues to believe, based on current science, that people are more likely to become infected the longer and closer they are to a person with COVID-19. The update acknowledges the existence of some published reports showing limited, uncommon circumstances where people with COVID-19 infected others who were more than six feet away or shortly after the COVID-19-positive person left an area. In these instances, transmission occurred in poorly ventilated and enclosed spaces that often-involved activities that caused heavier breathing, like singing or exercise. Such environments and activities may contribute to the buildup of virus-carrying particles.
On October 21, 2020, the CDC updated their definition of close contact to someone who was within six feet of an infected person for a cumulative total of 15 minutes or more over a 24-hour period starting from two days before illness onset (or, for asymptomatic patients, two days prior to test specimen collection) until the time the patient is isolated.
People can protect themselves from the virus that causes COVID-19 by staying at least six feet away from others, wearing a mask that covers their nose and mouth, washing their hands frequently, cleaning touched surfaces often and staying home when sick.
Learn more
This health brief on the clinical topics and innovations surrounding the SARS-coV-2 virus and COVID-19 disease was prepared by Buck’s Health Intelligence practice.
For more information, contact us at 866-355-6647 or talktous@buck.com.
| The information in this article is provided for general information purposes only and is not intended to address your requirements. While we will endeavor to keep the Information accurate, we cannot and do not guarantee the accuracy of the Information, and we accept no responsibility, and shall have no liability, for any loss or damage which may arise from using or relying on the Information. |
